Living With Myasthenia Gravis – An Interview With Dr. Kemi Olawaiye-Dampson
Myasthenia Gravis Awareness Month seems like the best possible time to not only educate about MG and spread awareness but also to bring hope and share stories of overcoming challenges and defeating the urge to give up. If there is one thing we at FindMeCure love doing for our readership it’s sharing patients’ personal experience, presenting stories with real-life happy endings without sugarcoating the hardship.
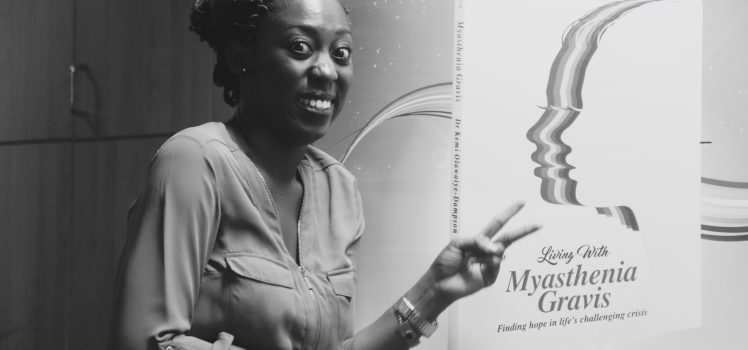
This is why today on the blog we’re sharing with you an interview that Dr. Kemi Olawaiye-Dampson gave for our blog. Her story is as touching as it is authentic and raw. Diagnosed with Myasthenia gravis shortly after the birth of her first child, Dr. Kemi Olawaiye-Dampson spirals into depression and self-pity. Feeling sorry for herself, however, did not improve her symptoms. After a long struggle, Dr. Kemi Olawaiye-Dampson finally had the realization that she could make lemonade out of the lemons she’d been given and give her experience meaning by sharing her story with people who need to hear it. This is how her book “Living With Myasthenia Gravis: Finding Hope In Life’s Challenging Crisis” came to be. Motivated to help as many people as possible, in 2016 Dr. Kemi Olawaiye-Dampson founded the non-profit organization Living free to live with the intention of spreading awareness and providing support to people living with MG.
Dr. Kemi Olawaiye-Dampson agreed to answer our questions and as always, we wanted to share useful information with you, so we asked some of the questions that would be of most interest to you. However, we’d like to remind you that everyone’s experience with MG is different and not everything you read here or elsewhere on the internet will apply to you or even make sense in your particular case. If something does hit close to home, address your concerns and questions with your doctor, maybe even share this interview.
- How did you get diagnosed and how much time did it take?
I got diagnosed in Saskatoon, Canada on May 27th, 2013 after having a myasthenic crisis. I had just had my first child after a very stressful pregnancy. I had thought the stressful part was over and it was mother-baby bonding time, but I guess life had a different plan for me. The happiest time of my life was immediately followed by the beginning of a dependent kind of life for me. During the weeks preceding my diagnosis, I had droopy eyes (which I had lived with for the greater part of my life), double vision, weakness in my arms, difficulty chewing and swallowing food including semi-solid and liquid diet. Then it progressed to weakness in my legs and eventually difficulty breathing. I needed help with doing everything including going to the bathroom, but the most saddening aspect for me was that I couldn’t care for my newborn. I ended up at the Emergency unit every week from the birth of my baby, till I got my diagnosis.
With regards to how much time it took, I would say it was long overdue considering I had been living with it for about 19 years without a definite diagnosis. However, it took 4 weeks for a definite clinical diagnosis to be made after the onset of that particular exacerbation and myasthenic crisis.
- What happened next? How long before you found the right treatment for you? How many different therapies did you try?
After the clinical diagnosis was made at the Emergency unit, I was admitted straight away to the Intensive Care Unit (ICU) that night. I was intubated the following morning, after which an ice test and a repetitive nerve stimulation tests were carried out on me. A blood sample for an antibody test was taken but the result came back 4 weeks later; it stated I was positive for the AntiMuSK type of MG with a titer of 2560. Of course, my neurologist didn’t wait for the antibody test report before starting treatment; he started me on IV Immunoglobulin (IVIG) and steroids. I had 2 courses of IVIG before my symptoms started to improve; well, the strength in my arms were the first to return. 2 weeks after I got admitted, I had to get a tracheostomy because the extubation failed twice after 5 hours and 7 hours respectively.
After 4 weeks at the ICU, I was finally able to walk and had successfully completed my trach-hood trials so I was no longer dependent on the ventilator. I was then transferred to the neuro-ward where I was started on Mestinon (Pyridostigmine). Unfortunately, this rather worsened my symptoms because I had increased secretions and breathing became difficult once again. After reading more about MG, we (my husband and I along with my doctors) discovered that Mestinon doesn’t work for AntiMuSK type of MG but rather Acetylcholine receptor type, so we discontinued it. I was then put on Imuran (Azathioprine) because the AntiMuSK MG responds better to immunosuppressants. I was eventually discharged on IVIG monthly, Imuran and Prednisone along with other supplements to manage the side effects of my medication. And oh, lest I forget, I was also discharged with a Percutaneous Endoscopic Gastrostomy (PEG) feeding tube in my belly because after 6 weeks with Nasogastric (NG) tube, I still could not even swallow my saliva without choking.
- Have you ever thought of trying treatments in development?
No, I haven’t. This is because I responded quite well to my combination of medication. I had the monthly IVIG for only 5 months because returned to Ghana IVIG was and still is not readily available. It’s also quite expensive. Also, I am currently in remission.
- How did you reach remission? Do you still take medicine while in remission?
If I tell you how I really reached remission, you might not believe me. Haha! I had my last major exacerbation in October 2015 after which I wrote my book “Living with Myasthenia Gravis”. My symptoms became relatively stable following this period; so, my Canadian neurologist, Dr. Paul Masiowski (who I am still in contact with till date) and I decided that I could taper my Imuran from 100mg daily down to 25mg daily. By this time, I was no longer on Prednisone, so I maintained the 25mg of Imuran for another 2 years. By the end of May 2017, I was completely off all medication, and I haven’t taken any medication since then, not even during my second pregnancy in 2017-2018. This doesn’t mean I don’t experience fatigue and weakness occasionally; it’s just that when they happen now, I just take time off to rest and I pace myself a lot.
- Do you supplement your treatment in any way? For example, a special diet, yoga, acupuncture, herbal medicine?
Hhhmmm… I would say I supplement my treatment but not in the way you think. I supplement with the word of God. I have to state that I believe in God and I have involved Him in everything I did during my journey with MG, so, unfortunately, I cannot talk about my story without mentioning this fact.
But to answer you, I tried yoga for a while but for some reason, I couldn’t continue. I try to exercise 3 times a week for about 10 mins; I walk my daughter to school and I use my gym bike. With respect to diet, I just try to eat healthy – salads, veggies, fruits, fresh home-made juice, and home-made smoothies.
Occasionally, I indulge myself… Haha… Ice-cream, pizza, Chinese food… Life is too short so I have to “happy myself” (as I like to say).
- What kind of assistance do you need from those around you on a bad day?
Wow! Bad days can really be bad. I usually need help with everything. I remember there were times my daughter (4 years old at the time) had to assist me in bathing, so she washed from my feet up to my waist while my husband washed my upper body. Haha! I can laugh about it now. MG made my daughter mature faster than her age-mates. There have also been times when my husband had to feed me like a baby.
- What do you wish family and friends of people with MG knew?
That’s a big question. I can write an epistle about this but I would try to summarize it.
First of all, WE ARE NOT LAZY!! And we are definitely not pretending. MG is an unpredictable disease; we might be fine one minute, and the next moment, we are experiencing a flare.
Secondly, if we disappoint you by canceling an outing, or not attending your party or paying you a visit, or even not picking up your call, it’s not because we’re being mean or inconsiderate. It’s because we are EXHAUSTED and too weak to talk.
Also, we already feel like a burden and a liability to you, so please be patient with us and try to remind us that you love us unconditionally.
I remember 2 years after I finally got my diagnosis, I felt like a burden to my husband (he never complained) because I felt/thought/believed that this was not what he bargained for when he married me. It bothered me for so long and I just needed reassurance and reaffirmation of his love.
- What made the biggest difference for you when it comes to MG? Was it mindset, was it your treatment team, your loved ones’ support, or something else?
I believe it was a combination of all of the above. My personal intro to MG began with a wonderful neurologist who was very patient and kind, and I believe that without him, this journey would have turned out completely different.
With regards to support, I have been blessed with a loving wonderful family. They have stood by me all through; cried with me when I needed it, prayed with and for me always, and made all the necessary sacrifices just to make life a little more comfy and pleasant for me. My husband has been and still is a rock. And oh, my daughter, ever ready to give me a hug when I cry because I am too exhausted. My children are the reason I keep on fighting daily; they are the reason I cannot ever give up.
My mindset also played a major role. Initially, I had a defeatist mindset about MG. I was always asking, “why me?” Then one day, I had to change my thought process, I had to start asking the right question. I realized that no amount of crying and wishing was going to take MG away, so I started to ask, “how can I live my life in spite of MG? I was then jolted out of the depression I had been sinking in. That was when my book “Living with Myasthenia Gravis” was written because I realized that my story could inspire others like me out there. Also, this new mindset led to the birth of the Living free to live Foundation which is dedicated to improving the quality of life of people living with MG through support group platforms and subsidized medication.
Now, to that “something else” part. I like to think of the “something else” as my Secret weapon or secret ingredient, and it’s my relationship with God. It keeps me going even when the road is rough and everything seems bleak. This secret ingredient of mine gives me hope daily.
- FindMeCure Foundation
I had heard of FindMeCure Foundation but I didn’t really know what they were about. I was intrigued and curiosity got the better of me, so visited their website. And boy, am I glad I did, because this has led to a partnership that I never even dreamed of.
Being a medical doctor and the Founder of a patient-focused Foundation, I believe that FindMeCure can make a difference in the lives of myasthenics living in Ghana. Managing MG worldwide is not an easy task, but even more difficult in our part of the world, owing to the poor availability and affordability of drugs needed to properly manage the symptoms.
My hope and belief is that this partnership between our 2 Foundations will take us a step closer to improving the quality of life of myasthenics in Ghana and the world as a whole.
If you have tried different treatments with no success so far or you feel like the side effects of your treatment outweigh the benefits, you can search for alternatives. Talk to your treatment team about clinical trials and search for a good fit on FindMeCure. You never know how close the next breakthrough in your treatment can really be.

